What's the trend
for controlling costs?
for controlling costs?
Healthcare costs have increased from
$1.2 trillion to $4 trillion over 20 years.
$1.2 trillion to $4 trillion over 20 years.
Family premiums are up 288%
over 20 years.
over 20 years.
Earnings have increased 103%
and inflation has risen 73%.
66% of bankruptcies are related to medical debt.
and inflation has risen 73%.
66% of bankruptcies are related to medical debt.
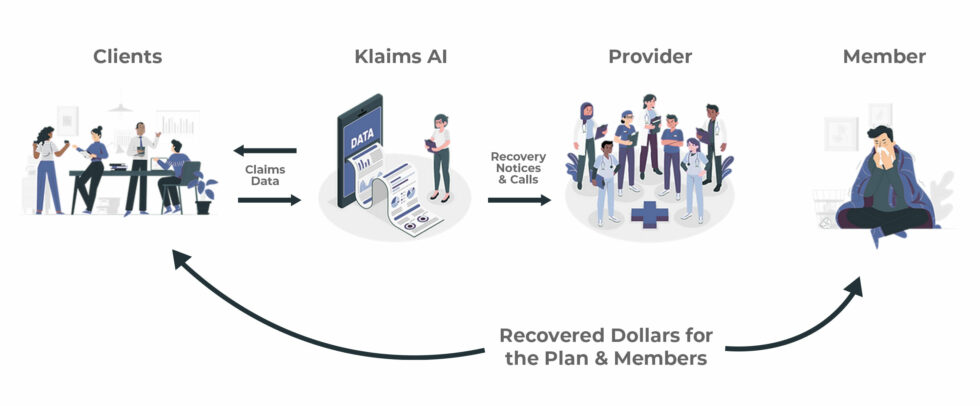
$325 billion is lost to medical overbilling
and fraud each year.
and fraud each year.
U.S. Department of Health & Human Services found that 22% of claims were paid improperly.
ERISA Risks:
Plan administrators and fiduciaries are ultimately responsible for protecting the plan from overbilling, fraud, waste, and abuse.